During recent sessions of JHF’s Fellowship on Death and Dying, participants discussed long-term care at the Jewish Association on Aging (JAA), hospice and end-of-life conversations at West Penn Hospital, and the experience of families and caregivers at the Good Grief Center. Through the fellowship, 43 graduate students—from 13 disciplines and six local universities—are preparing to have critical conversations about end-of-life care and exploring the medical, social, cultural, and spiritual aspects of end of life.
During the long-term care session at the JAA, Karen Feinstein presented an overview of the Foundation before the fellows toured the long-term care unit. After the tour, Mary Anne Foley, RN, MSN, JAA’s vice president of Home and Community Services, organized three small group discussions. JAA Director of Rehabilitation Services Phil Ricci, MOT, OTR/L, and Director of Social Services Nicole Morgan facilitated a conversation on long-term care. JAA Hospice Medical Director Stuart Chetlin, MD, Director of Professional Services Joy Rivett, Home Health and Hospice social worker Pearl Averbach, LCSW, and Bereavement Coordinator Jan Kellough discussed hospice. Rabbi Eli Seidman, JAA’s director of Pastoral Care, and Dan Leger, RN, of Sivitz Jewish Hospice & Palliative Care (part of the JAA’s continuum of senior care), led the spirituality discussion.
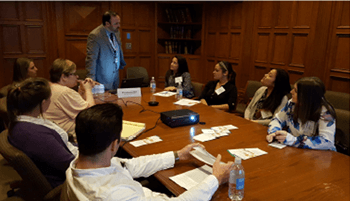 During the session at West Penn Hospital, the fellows toured the hospice unit with Lori Marshall, RN, Director of Allegheny Health Network Healthcare@Home, Hospice & Palliative Care; gained real-world insights on having end-of-life conversations with Judith Black, MD, medical director of senior products for AHN and Highmark and Randy Hebert, MD, chief medical officer of AHN Healthcare@Home; and were introduced to tools and technologies that can support advance care planning with Bill Gammie, MHA, president of AHN Healthcare@Home, Home Health, Hospice & Palliative Care.
During the session at West Penn Hospital, the fellows toured the hospice unit with Lori Marshall, RN, Director of Allegheny Health Network Healthcare@Home, Hospice & Palliative Care; gained real-world insights on having end-of-life conversations with Judith Black, MD, medical director of senior products for AHN and Highmark and Randy Hebert, MD, chief medical officer of AHN Healthcare@Home; and were introduced to tools and technologies that can support advance care planning with Bill Gammie, MHA, president of AHN Healthcare@Home, Home Health, Hospice & Palliative Care.
“There was variety in what we saw and plenty of chances for discussion,” one of the fellows commented following the session. “The importance of starting with a person’s values and goals—that lesson really came through for me.”
Later in March, the fellows visited Ursuline Support Services’ Good Grief Center and discussed the experience of family caregivers. Anthony J. Turo, executive director of Ursuline Support Services, explained that the Good Grief Center is the region’s first and only facility dedicated exclusively to bereavement education, resources, and referrals for people of all ages.
Nina Butler, EdD, led a discussion on caregivers’ and family members’ experience with death, dying, and grief. She noted the importance of creating a network of caregiver support to lessen the burden on a single family caregiver. Carol Frazer, LPC, a practice transformation specialist at PRHI, talked with the fellows about strategies to have end-of -life conversations with people when behavioral health issues are present. She also described the importance of self-care practices for healthcare professionals, so that they can manage their own feelings of grief and stress and best serve patients and families.
In early April, the fellows will synthesize their new experiences and skills to create action plans that improve end-of-life education, policy, and attitudes in their programs and communities.